TAVR procedures can cause
brain lesions, the largest of which can cause stroke
Risks in detail
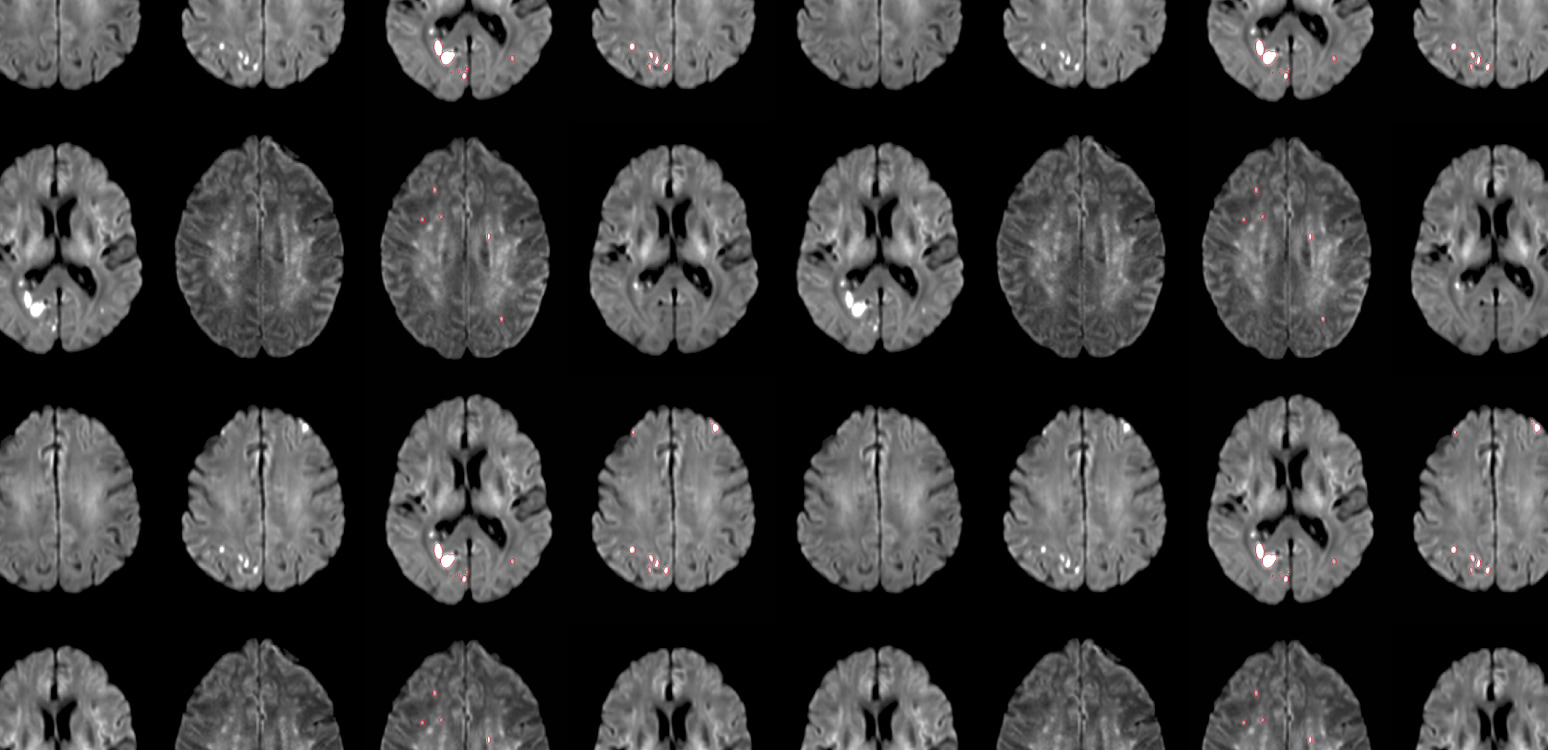
An acute lesion identified by diffusion weighted magnetic resonance imaging (DW-MRI) is generally a reliable signature of infarct and represents mostly permanent brain damage – sustained reversal is infrequent.3 These lesions are usually equally distributed in all major cerebral vascular territories except that of the Anterior Cerebral Artery.4,5
- Middle Cerebral Territory: 38%
- Posterior Cerebral Territory: 33%
- Cerebellar Brainstem: 27%
- Anterior Cerebral Territory: 2%
Silent brain infarcts, identified by DW-MRI, occur in the large majority of TAVR procedures with various associated risks.6
Although nearly all patients have many small lesions, many of these are not related to the release of debris and disappear after a short period of time. Cerebral Protection Systems serve to protect the brain from the debris that leads to the largest of these lesions, i.e., those that play a clinically meaningful role in developing a stroke and increase the risk of future stroke.
The number, size, and total volume of acute brain infarctions identified by DW-MRI are each associated with clinical ischemic strokes, disabling strokes, and worse stroke recovery in patients undergoing TAVR.7 However, large lesions that contribute to a total increased lesion volume (>500mm3) have specifically been correlated to higher rates of procedural stroke and increase the risk of future stroke ten-fold.1 These lesions are usually caused by debris that can be prevented from reaching the brain through the use of a CPS.
Large population-based studies demonstrate associations between MRI lesions and clinical stroke, mortality, and cognitive decline.10
Infarcts lead to brain volume reduction, but importantly are associated with with detectably lower cognition.1 Studies show that cognitive decline relates directly to loss of brain substance with progression of lesion burden.12
Cerebral infarcts have been linked to neurocognitive decline by affecting global memory function, dementia and hippocampal function and structure.13
Moreover, additional new infarcts are associated with more cognitive decline and an even higher risk for dementia than just having prevalent infarcts.14
Cerebral embolic protection (CEP) has become even more important as the TAVR patient profile is shifting to younger and lower risk patients.15, 22 12.2% of patients with aortic stenosis (AS) aged <65 years receiving aortic valve replacement were treated with TAVR, and 45% of patients in the US receiving TAVR were younger than 65 years of age.16
First-Generation CPS has Equivocal Clinical Results
Currently, there is only one cerebral protection system (CPS) that is commercially available both in the U.S.A. and Europe. The Sentinel™ device by Boston Scientific has been widely studied over the past decade, and its safety is undisputed. Despite this extensive experience, the approved intended use labelling does not mention that its use is associated with statistically significant reductions in either all stroke or the total volume of new cerebral lesions when assessed by DW-MRI.17
However, the per protocol analysis of the recent large meta-analyses (PROSPERO) demonstrates that Sentinel use, when used in appropriately selected patients and correctly deployed, is associated with a reduction in disabling stroke (control 1,3%, Sentinel 0,8% p=0.007).
- Lansky et al., Clinical significance of diffusion-weighted brain MRI lesions after TAVR: Results of a patient-level pooled analysis, JACC, Vol. 84, No. 8, 2024
- Kapadia et al., Protection against cerebral embolism during transcatheter aortic valve replacement, JACC, 2017;69:367–377
- Campbell et al., Journal of Cerebral Blood Flow & Metabolism, 2022;32:50-58.
- Arnold et al., Embolic cerebral insults after transapical aortic valve implantation detected by magnetic resonance imaging, JACC Cardiovascular Interventions, 2010 Nov, 3 (11) 1126–1132
- Wityk et al., Diffusion- and perfusion-weighted brain magnetic resonance imaging in patients with neurologic complications after cardiac surgery, JAMA Neurology, 2001;58(4):571-576
- Woldendorp et al. Silent brain infarcts and early cognitive outcomes after transcatheter aortic valve,implantation: a systematic review and meta-analysis, European Heart Journal 2021;42:1004-1015
- Kapadia et al, Cerebral embolic protection during transcatheter aortic valve replacement, NEJM 2022;387(14):1253-1263. doi:10.1056/NEJMoa2204961
- Seeger et al., Cerebral embolic protection during transcatheter aortic valve replacement significantly reduces death and stroke compared with unprotected procedures, JACC, 2017, Vol. 10, No. 22
- Kapadia et al., Cerebral embolic protection during TAVR, NEJM, 2023;388(7):669. doi:10.1056/NEJMc2215783
- Vermeer et al., Silent brain infarcts: A systematic review, Lancet Neurology 2007; 6:611-9
- Blum et al., Memory after silent stroke: Hippocampus and infarcts both matter, Neurology, January 3, 2012;78 (1) 38-46
- Schmidt et al., White matter lesion progression, brain atrophy, and cognitive decline: The Austrian stroke prevention study, Annals of Neurology, 2005, Vol.58, Issue 4: 610-616
- Vermeer et al, Silent brain infarcts and the risk of dementia and cognitive decline, 2003:348;1215-1222
- Sigurdsson et al., Incidence of brain infarcts, cognitive change, and risk of dementia in the general population: The AGES-Reykjavik Study (Age Gene/Environment Susceptibility-Reykjavik Study), Stroke, 2017, Vol. 48, No. 9
- Maxwell, TAVI use rising in young US patients, yet another analysis shows, TCTMD online, May 6, 2024
- Sharma et al., National trends in TAVR and SAVR for patients with severe isolated aortic stenosis, JACC, 2022, Nov 22;80(21):2054-2056
- Sentinel CPS Instructions for Use, https://www.bostonscientific.com/content/dam/elabeling/ic/51698992- 01A_SENTINELCPS_IFU_EN_s.pdf
- Jagielak et al., Safety and performance of a novel cerebral embolic protection device for transcatheter aortic valve implantation: The PROTEMBO C trial, EuroIntervention 2022;18:590-597
- Fezzi et al., Final report of the PROTEMBO C trial: A prospective evaluation of a novel cerebral protection device during TAVI, EuroIntervention, 2024;20:e264-e267
- Kodali et al., Cerebral protection in transcatheter aortic valve replacement: The SENTINEL study, JAMA 2015
- Nazif et al., Randomized evaluation of TriGuard 3 cerebral embolic protection after transcatheter aortic valve replacement: REFLECT II, JACC, 2021, Vol. 14, No. 5
- Praz F, Borger M, et al. 2025 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2025. doi:10.1093/eurheartj/ehaf194